Healthcare is arguably the only major industry in the world that hasn’t embraced automation — and it shows.
According to CMS, the annual U.S. spend on healthcare is nearly three trillion dollars (more than 17 percent of GDP), and yet the World Health Organization ranks our healthcare system below almost every other industrialized nation in the world. Despite all the money being spent, there is still pervasive inefficiency and frustration, with minimal relative value to the patient.
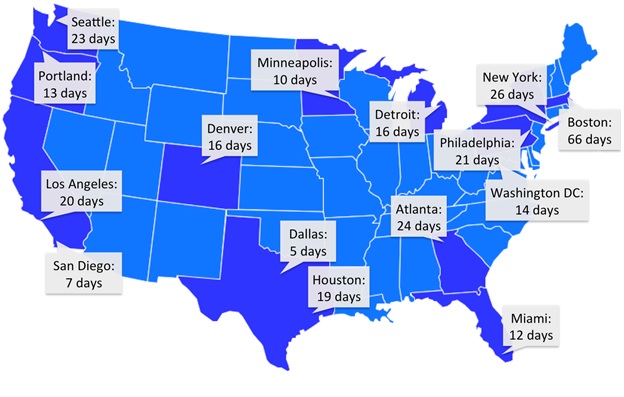
One obvious and difficult result of this lack of automation is the worsening primary care provider shortage. Average wait times for a patient to get primary care are staggering. In fact, among developed countries, only Canada has longer primary care wait times, and theirs are now improving.
This already untenable strain on the system is getting worse. It’s exacerbated by our population growth, the increasing average age of our population, and the introduction of new patients to the system under health care reform.
Every year, the U.S. population grows by more than 1.5 million, and every one of those new people needs healthcare. Additionally, the average age of our population is rapidly increasing. By 2025, the Census Bureau projects a 36 percent growth in the number of Americans over age 65. Not surprisingly, the elderly need more healthcare than the young.
VentureBeat will be discussing a variety of key health tech topics with industry innovators at HealthBeat 2014, Oct. 27-28 in San Francisco. Be sure to register.
Add to that the fact that our new healthcare reform legislation will help introduce 32 million previously uninsured Americans into the delivery system – most with a substantial backlog of care needs that will have a major per capita impact on demand for care.
On top of a system that’s already overburdened with patients, we’re also expecting more complex and time consuming care from existing primary care providers. The Affordable Care Act has helped catalyze a shift from a fee-for-service model to a capitated system of reimbursement. As part of that, primary care providers are now increasingly expected to provide care targeted towards preventing disease rather than just treating it. New activities like patient panel management and coordination of care are invaluable in delivering higher quality care but are also time-consuming and labor intensive for providers.
Increasing the number of doctors we’re training isn’t the answer. That would just be throwing more (expensive) bodies at the problem. Continuing to demand that providers work even harder isn’t a solution either. Over just a few decades, the number of patients that a provider sees daily has climbed from around a dozen to more than 20. If we continue to turn up the treadmill on our providers, quality of care will suffer.
The solution is building tools to help our providers work smarter. I like to draw an analogy to the agricultural revolution. As the urban population exploded, demand for food products increased and the world was faced with two options; get more farmers working harder with picks and shovels, or invent new, efficient ways of improving crop yields. The solution for our food shortage was not harder working farmers — it was the tractor. In healthcare we need to make a similar paradigm shift and explore out-of-the-box ideas that radically change the capacity of our healthcare system. We don’t need more doctors with picks and shovels. We need to be giving them a tractor to automate their work, doing things for them that we know they’ll need to do.
Solutions that will help automate healthcare processes aren’t just sought by patients and providers, either. With the explosion of wearable devices, manufacturers and delivery systems are struggling with how to get the right information from those devices in front of providers at the right time. Through well-designed software and clinical logic, device data about a patient’s blood pressure can be presented in a usable, actionable format when they are being treated for hypertension, and not when they have an earache.
Here are a few examples of automation tools that help deliver better, more efficient care:
SweetSpot Diabetes Care (recently acquired by DexCom) recognized that providers were drowning in data from simple, common glucometers. To help solve this problem, it automated the retrieval of data from numerous patient devices; managed, processed, and stored data in the cloud; and integrated the data into electronic medical records for provider use. It streamlined provider workflow and turned an ocean of glucometer data into usable clinical information. Endocrinologists using this system are able to quickly and easily review masses of information in seconds, quickly filtering to the most relevant data for any given patient or population.
WellBe helps to automate the peri-operative workflow, starting with the patient decision-making process and continuing through preadmission, surgery, and postoperative followup. Through automation, WellBe helps to standardize care processes, improving outcomes and lowering the total cost of care.
Kaiser Permanente’s Panel Support Tool or PST is an example of chronic disease automation. It automatically analyzes whole panels of patients, identifying gaps in care while keeping providers aware of evolving best practices and national guidelines. The key to this kind of automation tool is making sure that the information is automatically available, and only when the provider needs it. That way it supports the physician’s work rather than getting in the way.
Bright.md (Disclosure: This is the company I founded) automates up to 60 percent of primary care visit volume, reducing the provider time needed for those visits from 20 minutes down to less than two. That helps make getting high-quality care faster, more convenient, and less expensive for patients. It also increases margin for delivery systems and enables providers to practice at the top of their license. It also helps to expand provider capacity by 30 percent, making time available for the waves of patients waiting for care.
Fortunately, with the new ubiquity of EHR systems, the infrastructure for these kinds of services is already in place. EHRs are already beginning to evolve into the “operating systems” of the healthcare industry. Some progressive systems like DrChrono and Kareo are even building APIs and SDKs to help move that process along.
Now it’s time to build plug-in applications that expand EHR functionality and value. The same way that SalesForce helps automate CRM functions on a Mac or Windows computer, tools like SweetSpot Diabetes, WellBe, PST, and Bright.md help to automate evaluation, diagnosis, treatment, and documentation for providers on various EMR systems. And innovative delivery systems like CareMore are using these kinds of tools to support advanced clinical practices, with huge savings as a result.
U.S. funding for digital healthcare startups is expected to reach $6.5 billion by 2017, and given what a target-rich environment healthcare is, there’s room for even more growth. Still, some targets are higher value than others. Automation holds the keys to tremendous opportunity, in terms of patient experience, cost, and quality of care. The market for these kinds of tools is massive, the demand is growing, and the groundwork is already in place. It’s where I’m placing my bets. Where do you see the future of healthcare?
Ray Costantini, MD is co-founder and CEO of Bright.md, a virtual care solution that automates care and communication between physician and patient for faster, more convenient diagnosis and treatment.
VentureBeat's mission is to be a digital town square for technical decision-makers to gain knowledge about transformative enterprise technology and transact. Learn More