Skeptics of patient empowerment would be advised to tune into the real-time dashboard of Twine Health, which will be demonstrated for the first time publicly at HealthBeat, October 27-28.
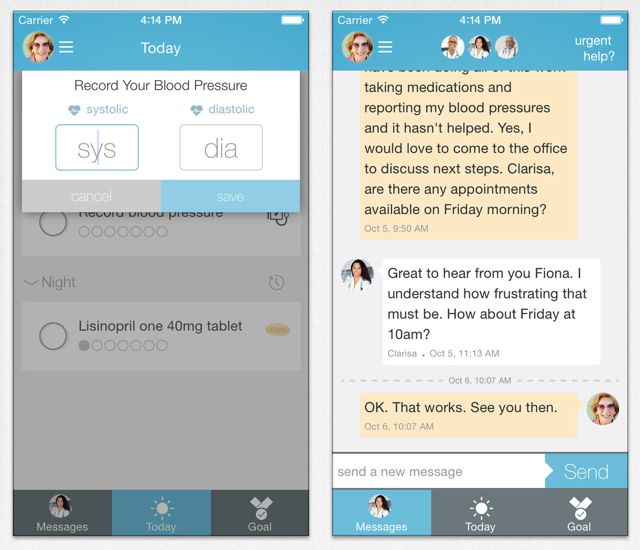
The cloud-based platform is designed to put some of the management of chronic disease in the hands of patients. It’s based on a coaching model that sees the patient as apprentice in their own health care. With clinicians and patients working together using synchronized apps, they create plans to reach important health goals decided on together.
“There’s a new level of transparency in health care,” explains Twine Health co-founder and CEO John Moore. “It’s time to shut up and show it for all to see.”
The platform is in place in six U.S. clinics working with hypertension patients.
Twine Health outperformed office visits
The Twine approach was tested in a six-month randomized control trial, which compared the progress of patients who see their providers only in office visits, with those using Twine Health. In the office-visit group, 30 percent of patients reached their blood pressure goal at a cost of approximately $250 per patient per year. In the Twine Health group, 100 percent of patients reached their blood pressure goal at a cost of about $75 per patient per year. The Twine group also achieved its goal in a quarter of the time of the office-visit group.
At HealthBeat, Moore will be sharing a live dashboard showing aggregated statistics such as how many patients are using the platform, patients’ progress toward their targets, and how much clinical time is being spent. He doesn’t believe technology solutions should live in a black box where no one else can learn. By publishing results live to the web, exposing Twine Health’s advances and even its mistakes Moore sees the value in inviting the community to comment to continually get better at empowering patients in their care.
“Patients are smart,” Moore says. “We’re holding them back by being so afraid of giving them more freedom and it just doesn’t make any sense.” He goes on to explain that patients live in the real world where they make decisions on their own every day. It’s far better for them to be making smart choices enabled by a collaborative partnership, than left alone and simply given an appointment to show up for an office visit where the physician maintains control.
Personal, real-world, and human
Moore attributes the success of the platform to three essentials:
- The platform allows patients to create very personalized care plans. He differentiates this from cookie-cutter automated protocols on the market. “Patients weigh the risks and benefits of different choices and what they want to achieve,” he explains. “It’s their personal story.”
- The platform moves with the patient into the real world. As Moore explains, it’s not just about following a patient for a few weeks after they’ve been in the hospital to prevent a readmission. It’s about staying with a patient for the long-term as they manage their condition in their every-day lives.
- It’s human. Moore sees technology only as a tool to human connection. For him, the platform represents a thoughtful balance between the technological and the human. “It’s not that we don’t use technology wisely to do automation and calculations and things like that, but the patient experiences Twine as fundamentally human through connecting with that other person.”
Covering the full spectrum of chronic disease within a year
Although Twine’s been in the corporate medical world for just a year, it began life at the MIT Media Lab. Over six years there, Moore and his team did research using the platform with HIV, diabetes, and hypertension patients. Prototypes were used to help Parkinsons Disease, congestive heart failure, epilepsy, and post surgical care patients. Within another year, Twine hopes to be covering the full spectrum of chronic disease including these and other diseases such as COPD (chronic obstructive pulmonary disease), CHF (congestive heart failure) and asthma.
Movement toward that goal is being hastened by the move to value-based payment compensation models from fee-for-service. “The folks we work with typically are making a commitment to improving their outcomes and cutting their costs because they’re on a value-based compensation model — or they see that coming,” says Moore.
However, old attitudes die hard. When it comes to patient-generated data, Moore says that certain clinicians are afraid that patents will falsify data, or misinterpret data, or make wrong decisions based on that data. He also asserts firmly that a decade of research shows those fears are entirely unfounded.
In fact, he says, “There’s plenty of evidence to show that we’re actually doing more harm to patients by not embracing their ability to contribute.”