This sponsored post is produced by Better Health East Bay.
Our nation’s healthcare system often struggles to meet the needs of the community. It isn’t as efficient as it could be, often slow to adapt to changing needs. As a result of the Affordable Care Act, there are many more insured patients in need of care, putting a strain on an already fragmented system. With some doctors now turning away patients, heading to the emergency room for what is typically considered non-urgent care has become all too common.
Not only does this overburden our ERs with an influx of non-urgent needs, but the costs are skyrocketing. It’s an unsustainable system bound to fail.
The most vulnerable account for the most costs
Nowhere in California is this more of a crisis than across the bridge from San Francisco, in the East Bay region, where 34 percent of the more than 2 million residents are vulnerable to serious health issues. And, in communities like Oakland and Berkeley, where complex health issues are common, the most vulnerable patients account for the majority of the costs and require the most resources. In fact, 70 percent of those with less urgent needs live within just a mile of a quality, affordable health center, but still opt for care at the ER. The question is, “why?”
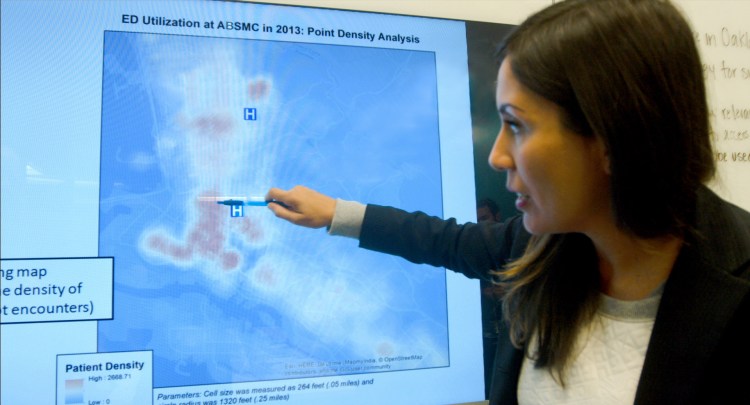
Hotspotting: identifying where the need is most
Today, Alta Bates Summit Medical Center in Berkeley and Oakland is tackling that issue and many others. The hospital is one of only six in the U.S. to pilot the groundbreaking hotspotting “super-utilizer” program, pioneered by Dr. Jeffrey Brenner in Camden, New Jersey. Dr. Brenner’s work, which earned him a MacArthur “Genius” Award, uses patient data to identify high-risk locations where health problems are clustered, services are scarce, and people have the hardest time getting primary care.
Using state-of-the-art technology and GIS mapping tools to better understand and predict the healthcare patterns and needs of these most vulnerable populations, the team at Alta Bates Summit is building a comprehensive network of care that doesn’t exist today. Built into the system is the ability to redirect patients to quality and convenient care resources, including access to a specially-trained group of case managers for personalized support and follow-up.
By strengthening the safety net throughout the community served by Alta Bates Summit, their goal is to reduce non-urgent visits to emergency rooms, controlling escalating costs, while greatly improving health outcomes.
Out of the ER and into the streets
An example of putting hotspotting into action is a partnership with the Berkeley Free Clinic. Using patient data from Alta Bates Summit, the Clinic’s mobile van can better identify clusters – hotspots – where the most vulnerable Berkeley populations live and then get medical resources directly to those patients quickly and more efficiently. It’s a simple idea and a common sense approach to going where the needs are greatest, to help people get the right care affordably, where and when they need it.
Redesigning the healthcare system is a massive undertaking, but it is achievable, with the right amount of innovation and investment. Done well, we have the chance to change the face of healthcare forever and for the better.
Jim Hickman is CEO of Better Health East Bay.
 This post is brought to you by Better Health East Bay.
This post is brought to you by Better Health East Bay.
Sponsored posts are content that has been produced by a company that is either paying for the post or has a business relationship with VentureBeat, and they’re always clearly marked. The content of news stories produced by our editorial team is never influenced by advertisers or sponsors in any way. For more information, contact sales@venturebeat.com.